This activity is provided by Med Learning Group.
This activity is supported by an independent medical education grant from Regeneron Pharmaceuticals, Inc.
Copyright © 2024 Med Learning Group. Built by Divigner. All Rights Reserved.
Maintaining Mental Health
Maintaining Mental Health
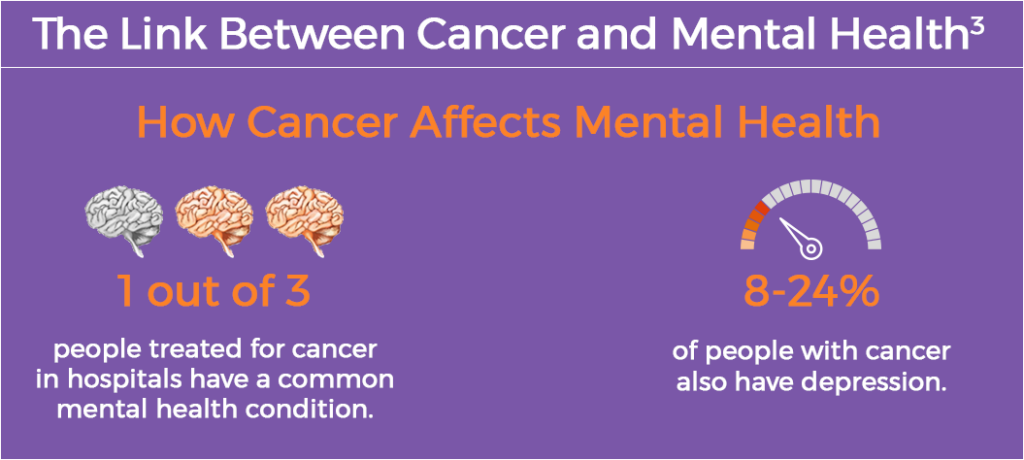
A diagnosis of cancer impacts not only physical health but also mental health.1,2 Anxiety, depression and stress are commonly experienced by patients, related to screening, awaiting test results, diagnosis, treatment, recurrence and navigating the care plan.1,2 It is estimated that one in three patients with cancer treated in hospitals also have a common mental health condition (ie, affective and anxiety disorders), with as many as 8% to 24% of patients with cancer having depression.3
Healthcare providers play an important role in addressing their patients’ mental health.2 Patient-provider conversations should focus on both the physical and mental impact of cancer and its treatment.2 It is also important to monitor patients with cancer for signs and symptoms of mental health issues, as some may overlap with side effects related to cancer and treatment, such as loss of appetite, weight changes and sleep disruption.1,2 Patients with anxiety or depression may be less likely to follow their treatment plan and may be more likely to miss appointments.2 Research has shown that veterans with lung cancer who received mental health treatment and social support lived longer and were more likely to receive optimal treatment for their cancer at any stage.4
Burnout Among Oncology Providers
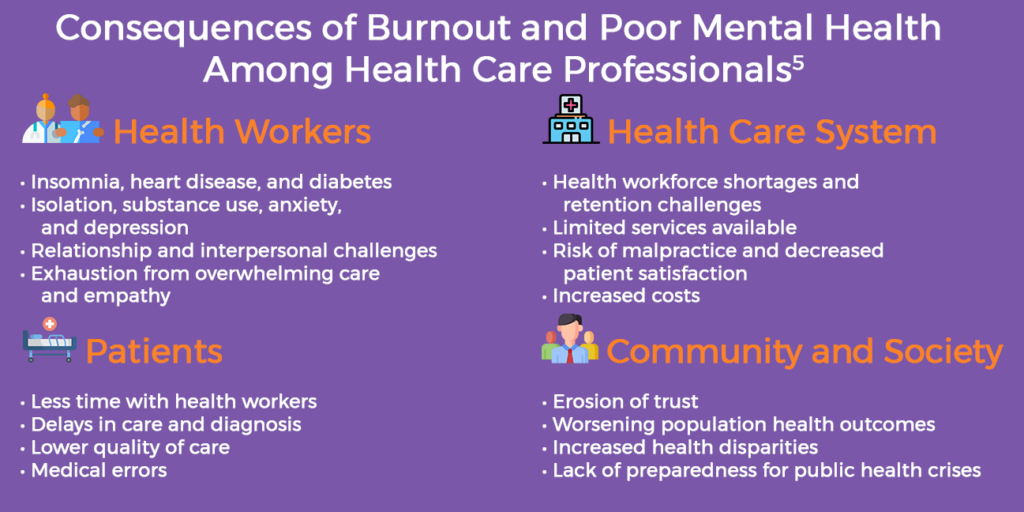
Burnout and wellness are pressing issues in medicine today.5 Many healthcare professionals work in demanding environments that impact their physical, emotional and psychological well-being.5 It is estimated that 50% of physicians will experience burnout at some point during their careers.6 Healthcare workers are at increased risk for burnout and mental health issues due to a spectrum of societal, cultural, structural and organizational factors, such as excessive workloads, administrative burdens, scheduling challenges and lack of support.5,6 This includes oncology providers, due to the demands of delivering complex cancer care.6,7 In a recent American Society of Clinical Oncology (ASCO) survey on burnout and career satisfaction, 45% of US oncologists reported feeling symptoms of burnout.8 Moreover, the unique challenges of practicing oncology, including continuous exposure to life-threatening illness and grief, increase risk for depression and suicide among providers.6
Occupational and personal consequences of burnout and mental health issues were further exacerbated by the COVID-19 pandemic, due to fear and risk of infection, disruptions in care, telemedicine, loss of social support, and delays in cancer screening, diagnoses, and treatment.9 Research from the American Medical Association (AMA) revealed that 63% of physicians reported symptoms of burnout at the end of 2021, an increase from 38% in 2020.10,11
Together, these factors can affect cancer care delivery and the well-being of providers and patients under their care.6 These challenges have also led some providers to leave the health workforce early.6
Addressing Mental Health
Addressing emotional and mental health is a vital part of cancer care.12 Screening for mental health has become a standard of cancer care across most institutions and facilities.13 Individual and group counseling that focuses on thoughts, feelings and behaviors are often recommended for patients with cancer.13 Other strategies for patients may include1-4,12,13:
Medication
Meditation and/or yoga
Journaling
Support from the cancer care team, other healthcare providers, family and friends
Breathing exercises
Exercise, when appropriate
For providers, in addition to the strategies above, large-scale changes are needed to address mental health. The ongoing crisis of burnout and mental health is a focus of many organizations, systems, professional societies and beyond. Potential interventions to combat burnout may include5,6,10,11:
References
- American Cancer Society. Emotional, Mental Health, and Mood Changes. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/emotional-mood-changes.html
- Georgetown University School of Nursing. Managing Mental Health After Cancer Diagnosis. https://online.nursing.georgetown.edu/blog/cancer-mental-health/
- Mental Health America. Cancer and Mental Health. https://www.mhanational.org/cancer-and-mental-health
- National Cancer Institute. Study Links Mental Health Treatment to Improved Cancer Survival. https://www.cancer.gov/news-events/cancer-currents-blog/2020/lung-cancer-treating-mental-health-longer-survival
- U.S. Department of Health and Human Services Office of the U.S. Surgeon General. Current Priorities of the U.S. Surgeon General. Health Worker Burnout. https://www.hhs.gov/surgeongeneral/priorities/health-worker-burnout/index.html
- Hlubocky FJ, Taylor LP, Marron JM, et al. A call to action: Ethics committee roundtable recommendations for addressing burnout and moral distress in oncology. JCO Oncol Pract. 2020;16:191-199.
- McFarland DC, Hlubocky F, Susaimanickam B, O’Hanlon R, Riba M. Am Soc Clin Oncol Educ Book. 2019;39:590-598.
- ASCO Connection. Physician Wellness and Professional Burnout. https://connection.asco.org/physician-wellness
- Hlubocky FJ, Back AL, Shanafelt TD, et al. JCO Oncol Pract. 2021;17:e427-e438.
- American Medical Association (AMA). Measuring and Addressing Physician Burnout. October 20, 2022. https://www.ama-assn.org/practice-management/physician-health/measuring-and-addressing-physician-burnout
- Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic Mayo Clin Proc. 2022;97:2248-2258.
- Granek L, Nakash O, Ariad S, Shapira S, Ben-David M. Strategies and barriers in addressing mental health and suicidality in patients with cancer. Oncol Nurs Forum. 2019;46:561-571.
- Donovan KA, Grassi L, Deshields TL, Corbett C, Riba MB. Epidemiol Psychiatr Sci. 2020;29:e85.
All URLs accessed February 9, 2023